Hormonal coil
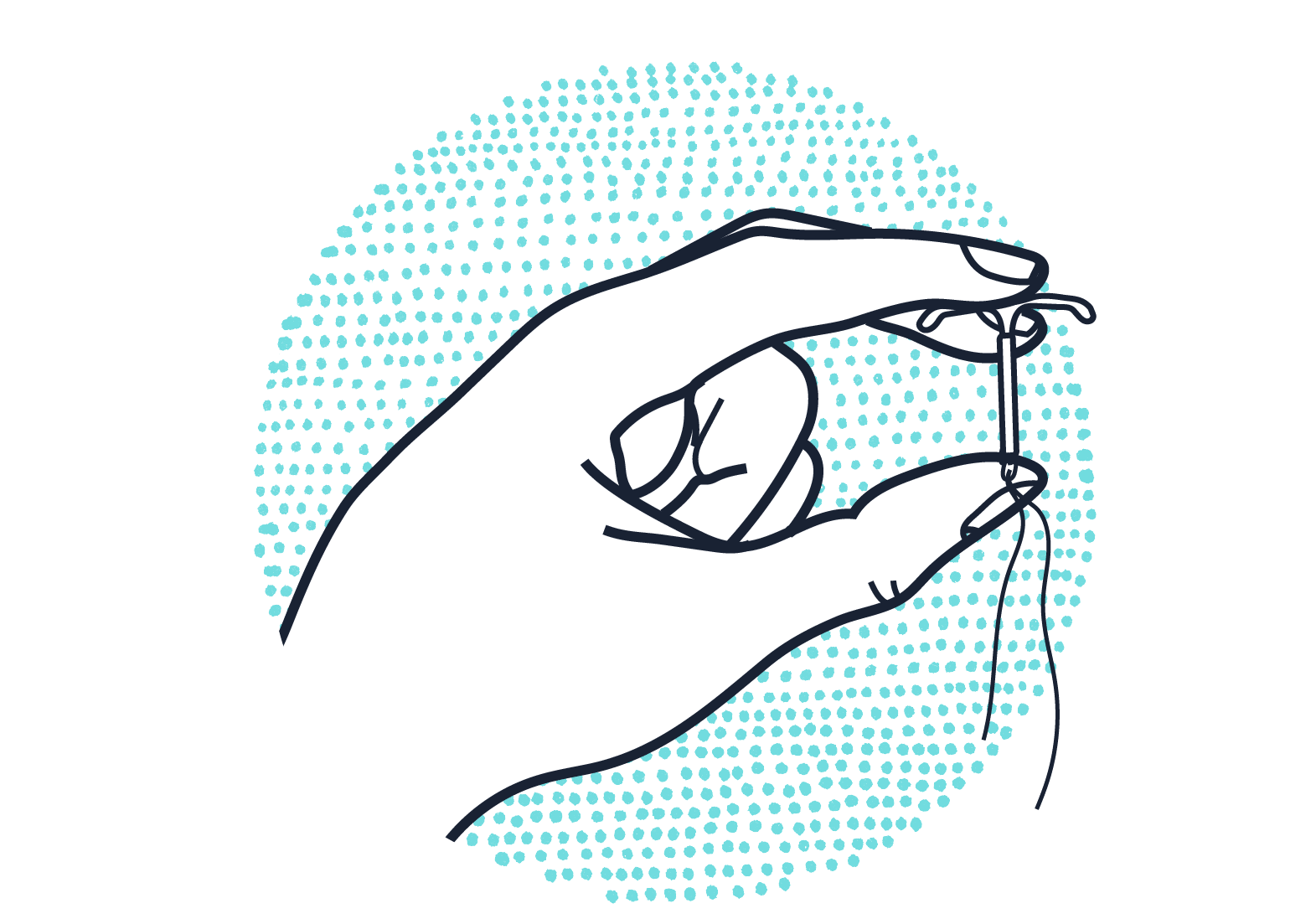
The hormonal coil sits in the uterus for up to 8 years, constantly releasing small amounts of the hormone progestogen, a synthetic hormone that mimics the body’s natural progesterone. It’s a highly effective contraceptive that reduces bleeding to little or nothing in most people.
frequency: fit and forget
effectiveness: over 99%
STI protection? no
periods: reduces bleeding
What you need to know about the hormonal coil
It’s the most effective contraceptive, more effective than sterilisation. And it can last longer than any other method. It needs to be fitted by a clinician with specialist qualifications but it’s easy for non-specialist clinicians to remove, after which your fertility returns to what is normal for you.
How does the hormonal coil work?
It mainly works locally in the womb, slowly releasing progestogen that doesn’t move through the whole body like it would with a pill. The progestogen in the womb area still thickens cervical mucus, stops sperm from entering the womb and thins the womb lining so a fertilised egg can’t implant.
Getting started with the hormonal coil
It’s fitted by someone with specialist training. Some people find it painful, others don’t. It's effective 7 days after it's fitted.
Health benefits, risks and side effects of the hormonal coil
The most important side effect is that it reduces bleeding – and usually period pain – to little or nothing. The hormone mainly stays in and around the womb (uterus) so you may get fewer hormonal side effects in other parts of the body.
Do you need help with something else?
Find sexual health services near you
Get sexual health advice from the experts






